Solutions Improved Administrative Efficiency on Denied Claims

Challenge
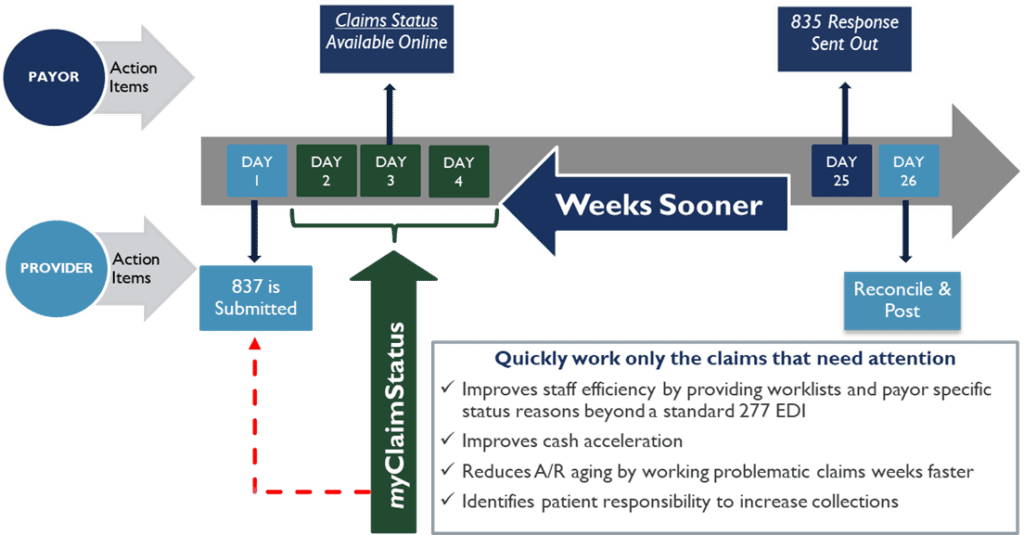
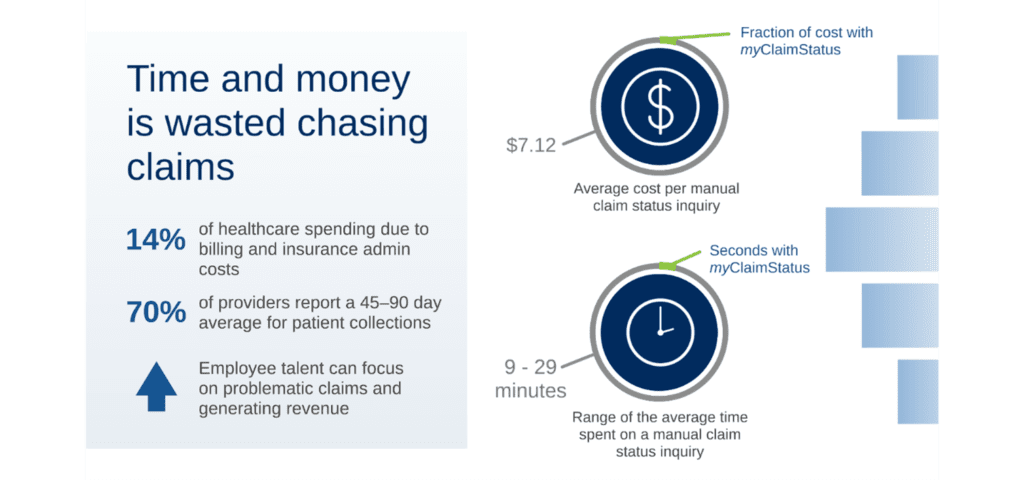
Hospitals typically wait weeks from bill submission to be advised of payment status and amount. This delay negatively impacts when a hospital can bill a patient or appeal a denied claim.
Solution
myClaimStatus provides hospitals with significant workflow efficiencies and the ability to jumpstart their A/R follow-up through our proprietary robotic process automation.
- Accesses payor databases eliminating phone calls & manual searches for claim status
- Receives 837s and automatically queries payor websites
- Returns actionable claim status info immediately when available
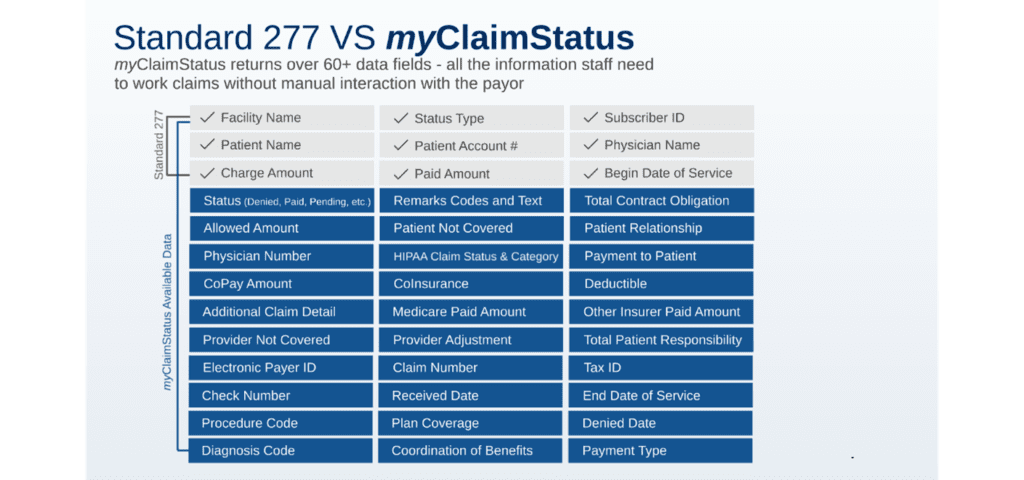
- Gives all available claim info to provider unlike 277s